The Zika virus
This is the first of a three part series of briefs dealing with the Zika virus. It will discuss its identification and spread, correlating the spread with the incidence of Aedes mosquitoes. The second will describe the new health implications for humans, and the third will discuss what the World Health Organization and the United States Centre for Disease Control are currently doing to keep the infection rate under control.
History
The Zika virus was first identified in a rhesus monkey in the Zika forest of Uganda in 1947. The next year, the virus was recovered from an Aedes Africanus mosquito caught in the forest. The first human infections were detected in Uganda and Tanzania in 1952 through serological studies, though it was not established until 1964 that the virus causes human disease. From the 1960s, human infection was found across equatorial Africa and the virus was isolated from more than 20 mosquito species, mainly in the genus Aedes. . From 1969 the virus was also found in equatorial Asia, including India, Pakistan, Malaysia and Indonesia. The two most prominent species are Aedes aegypti (the yellow fever mosquito) and Aedes albopictus (the Asian tiger mosquito) which transmit the viruses that causedengue fever, yellow fever, West Nile fever, chikungunya, eastern equine encephalitis, and Zika virus. In both regions, seroprevalence studies indicated widespread exposure in humans, but up to 2007 only 14 cases of illness had been documented worldwide. The incidence of illness must have been much higher but, since symptoms are usually mild and the disease easily confused with dengue and chikungunya, little attention was paid to it.
In 2007, the virus reached the island of Yap in the Federated States of Micronesia, causing 185 cases of suspected Zika disease. An estimated 73% of the population over three years of age were found to be infected. No evidence of viral mutation was found, and it was suspected that the higher reported incidence of the disease in Yap may have been caused by lack of population immunity in Micronesia and the under-reporting of cases before 2007.
In 2008, it was discovered that the virus could be sexually transmitted as well as through infected mosquitoes, and there is a risk of transmission via transfusions. In 2012, two distinct lineages of the virus were distinguished: African and Asian. There is further differentiation within each lineage. It appears that Zika in Latin America belongs to the Asian lineage[1]. In 2013 and 2014, the virus spread to other Pacific Islands and it has now been found in 72 countries, as indicated in Figure 1, published by the WHO in early September 2016. This map represents new Zika notifications since 2013. The darker the blue, the more recent the notification. Circulation of Zika virus in Thailand, Cambodia and Lao People’s Democratic Republic (marked in dark grey) started before 2013. Countries where sexual transmission occurred are not represented in this map. Available information does not permit measurement of the risk of infection in any country; the variation in transmission intensity among countries is therefore not represented on this map. Zika virus is not necessarily present throughout the countries/territories shaded in this map.
Figure 1. Global spread of Zika virus, 2013-2016
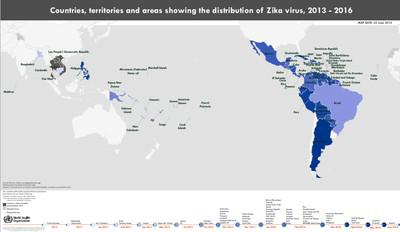
Figure 2 maps the probability of finding the Aedes aegypti and Aedes albopictus mosquitos.
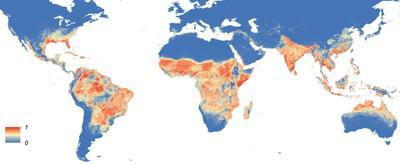
Aede aegypti

Aede albopictus
Source: Kraemer, M. U. G., et al., 2015. The global distribution of the arbovirus vectors Aedes aegypti and Aedes albopictus
Note: The probabilities vary from zero (blue) to one (red)
Figure 2 indicates the possibility of Zika infection in a number of countries which have not yet reported it. Recent research in Brazil has shown that the Culex mosquito may also transmit Zika.
On 6 July 2016, the Department of Health advised travellers that there is no threat of contracting the Zika virus in South Africa, noting that it has not been found south of Uganda[2]. The National Health Laboratory Service points out that the typical African subspecies tends not to bite humans[3], and that local Aedes aegypti mosquitoes have very limited flight ranges (measured in a few metres) and tend not to enter buildings. The Aedes aegypti mosquito has been present in South Africa for many years, without any case of Zika infection being reported. Professor Leo Braack of the University of Pretoria reports that it is common in certain areas of South Africa, especially in the warmer, northern areas, such as along the KwaZulu-Natal coastline, but it is also found elsewhere, including some urban areas. This species typically lays its eggs in small volumes of water, such as you would find in discarded tin cans, blocked roof gutters, pots of stored water in rural areas and bird baths that are not flushed regularly, or on the leaf axils of Strelitzia nicolae (“banana trees”). He points out that viruses transmitted by insects usually have an animal that functions as an amplifier host, in which the virus multiplies to sufficient levels to provide an important source of infection. Such an animal is either absent or the virus has never been introduced to a susceptible amplifier host in this country.
However:
1. The Zika virus was found in a visitor from Colombia in February 2016.
2. There have been no serological studies in South Africa with the Zika disease having very little reported cases in Africa, and the virus has spread fast internationally.
The probability of a Zika outbreak in South Africa may well be low, but it cannot be discounted completely.
Conclusion
The Zika virus is found mainly in tropical areas, but it is found in sub-tropical areas as well. The list of countries reporting its presence is growing, and the possibility of its spread through human to human contact needs to be kept in mind. What is more, the list of conditions which may present themselves in infected people is growing. This will be the subject of the next brief.
[1] See Antione Enfissi et al, Zika virus genome from the Americas, Lancet, 16 January 2016
[2] But note the Tanzanian case mentioned above
[3] The WHO finds that Aedes aegypyti mosquitos prefer to bite humans over animal hosts
THE ZIKA VIRUS II - ZIKA DISEASE
The first brief in this series described the geographical distribution of the Zika virus. This brief deals with the symptoms which result from infection.
Introduction
The Zika virus continues and has been found in 70 countries so far. The Zika illness is generally mild, with symptoms including a slight fever or rash, appearing a few days after a person is bitten by an infected mosquito. Many will not develop any symptoms at all, but some may also suffer from conjunctivitis, muscle and joint pain, and feel tired. The symptoms usually last from 2 to 7 days. They can be treated with common pain and fever medicines, rest and plenty of water.
Diagnosis is based on symptoms and the person’s recent history (e.g. mosquito bites, or travel to an area where the Zika virus is present). Laboratory testing can confirm the presence of the Zika virus in the blood. However, the diagnosis may not be reliable, as the virus could cross-react with other related viruses such as the dengue, West Nile, yellow fever and Japanese encephalitis viruses, carried by the same mosquitoes.
Complications
However, more serious effects of Zika infection have been identified recently. There is now scientific consensus that infection in a pregnant mother can cause congenital brain abnormalities, including microcephaly – birth with an unusually small head – in her infant. In January 2016, ophthalmological abnormalities were reported in three children with microcephaly and cerebral calcifications detected by CT scans and presumable intrauterine Zika infection. More recently, the WHO has reported a wider range of manifestations in infants: craniofacial distortion, spasticity, seizures, irritability, brain stem dysfunction, cortical disorders and ventriculomegaly (enlargement of the ventricles in the brain).
There is also consensus that infection can trigger Guillain-Barré syndrome. Guillain-Barré syndrome is a disorder in which the body's immune system attacks part of the peripheral nervous system. It creates weakness, first in the legs, and then in the arms and upper body. In severe cases, it can result in almost total paralysis, and is life threatening. It can last for several weeks. Most individuals recover from even the most severe cases of the syndrome, although some continue to have a certain degree of weakness. But between 3.5 and 12% of patients die from complications during the acute phase: sepsis, pulmonary embolism or cardiac arrest.
The Zika virus can cause other neurological syndromes: meningitis, meningoencephalitis, myelitis and Fisher syndrome. Meningitis is a serious disease in which there is inflammation of the meninges, caused by viral or bacterial infection, and marked by intense headache and fever, sensitivity to light, and muscular rigidity. Meningoencephalitis simultaneously resembles both meningitis and encephalitis, which is an infection or inflammation of the brain. Myelitis is inflammation of the spinal cord. Fisher syndrome is characterized by impairment of eye movements, abnormal coordination and loss of tendon reflexes.
In rare cases, the Zika virus can cause uveitis (inflammation of the middle tissue of the eye) which can lead to pain, blurred vision and, in severe cases, blindness.
Recent research
Fundamental research on the Zika virus and its effects has started to appear. The May 2016 edition of Science Magazine reported that experiments with mice show precisely how the virus slows foetal growth, damages the brain and leads to miscarriage. Studies of monkeys naturally infected with Zika are under way.
A Science News Bulletin from Rockefeller University on 18 August 2016 indicated, based on mice studies, that certain adult brain cells may be vulnerable to infection, as well as brain cells in foetuses. Among these are populations of cells that served to replace lost or damaged neurons throughout adulthood. These cells are also thought to be critical to learning and memory. Particularly vulnerable are the sub-ventricular zone of the anterior forebrain and the sub-granular zone of the hippocampus. The hippocampus is situated in the medial temporal lobe of the brain. It is just below the amygdala which is responsible for detecting fear and dealing with emergency events.
The 6 September 2016 edition of LiveScience reported that mice studies show that genetic material from the virus can find its way into tears, raising the possibility of infection through contact with them.
Findings from mice and monkeys, though suggestive, do not automatically imply the same effects in humans. The vulnerability of human foetuses to the Zika virus is clearly established, but it may well be that infection has long term degenerative effects on children and adults as well.
Conclusion
The adverse impact of the Zika virus may stretch well beyond any mild immediate illness resulting from infection. In the view of the WHO, Zika virus infection and its associated congenital and other neurological disorders continues to be a Public Health Emergency of International Concern.
The final brief in this series will discuss what the World Health Organization and the United States Centre for Disease Control are currently doing to keep the infection rate under control.
THE ZIKA VIRUS III - THE WORLD HEALTH ORGANIZATION AND THE CENTRE FOR DISEASE CONTROL
This is the last Brief in a three part series dealing with the Zika Virus. It discusses what the World Health Organization (WHO) and Centre for Disease Control (CDC) is currently doing in order to cope with the Zika epidemic.
Introduction
The WHO and CDC have increased the measures that they are taking to deal with Zika. The WHO releases regular situational reports and the CDC has released an interim response plan.
The WHO situational reports
Each week the WHO issues a situational report. The report sets out new notifications of mosquito-borne and person-to-person transmission of the Zika virus, and of associated diseases. It contains operational updates from WHO regional offices, and it reports key research findings. The report of 8 September 2016 contains the following information:
1. It was noted that Malaysia had reported a locally acquired mosquito-borne Zika infection in the last week, a new development for that country.
2. The WHO Regional Office for the Americas has conducted workshops on clinical management of neurological complications in Barbados. A technical mission to Brazil for laboratory assessment and strengthening of Zika diagnostic capacity of State laboratories was completed in August. WHO facilitated two meetings in Panama with regards to the updating of the strategic plan for vector surveillance and control. In Columbia and El Salvador there were Mosquito Awareness Week programmes. In Haiti there were three train-the-trainer workshops on epidemiological surveillance of Zika and its complications in August. WHO has provided technical support to the Brazilian Ministry of Health to ensure that the Summer Paralympic Games are as safe as possible.
3. An analysis of the Zika virus cases in Singapore indicates that the virus belongs to the Asian lineage, evolving from the South East Asian strain and is likely to have surfaced in South-East Asia first.
4. There have also been meetings conducted by the Emergency Committee looking into the Zika virus and its infection and associated congenital and other neurological disorders which continue to be a public health emergency of international concern. WHO has also been able to establish that the Zika virus infection in pregnant women is the cause of the congenital brain abnormalities including microcephaly and that the Zika virus can trigger the Guillain-Barre’ Syndrome. WHO issued a revised guideline on the prevention of sexual transmission which was published on 6 September 2016.
The CDC response
The CDC has developed a 10 step programme for infected areas to implement.
Step 1: Vector surveillance and control.
This consists of identifying vectors[1] in areas where the Zika virus is present, surveying their incidence and developing and implementing plans for their control, especially in areas where the Aedes mosquito is found. This step also involves educating communities on self-protection.
Step 2: Public Health Surveillance and Epidemiological Investigation
The goals are to ensure that adequate diagnosis and reporting of the Zika virus cases occurs, and to monitor epidemiologic trends in transmission, distribution and severity.
The activities are to determine if systems and procedures are in place to identify confirmed Zika cases. This can be done by considering looking at:
- Symptomatic infection
- Problems in pregnant women
- Reproductive or congenital outcomes including microcephaly
- Guillain-Barré syndrome
- Infections as a result of blood transfusions
- Infections transmitted sexually
Step 3: Laboratory testing and support services
The goal is to ensure that state and territorial departments have the support needed to adequately test specimens from suspected Zika cases.
This entails determining which laboratories in a particular place are capable of conducting molecular tests or antibody tests for the Zika virus infection, to put in place mechanisms for testing, and training health care providers about submitting specimens.
Stage 4: Prevention of Sexually Transmitted Zika virus Infections
The goal is to focus on reducing the risk of sexually transmitting the Zika virus by providing guidance to the public regarding the risks.
The actionable steps are to educate the public as well as health care providers as to the risks of sexual transmission of the Zika virus as well as to promote the following of the guidelines for prevention and transmission as issued by the CDC.
Step 5: Prevention of Blood transfusion- transmitted Zika Virus Infections
The goal is to reduce the transmission of the Zika virus through blood transfusions in areas with an outbreak of Zika. The actionable steps here are to co-ordinate with surveillance partners in order to investigate when the Zika virus may have infected blood products or transfusions in local blood centres and transfusing health care facilities, and to introduce testing of blood products for the Zika virus.
Step 6: Maternal and Child Health Surveillance and Response
The goal is to ensure that infection during pregnancy is prevented as well as to ensure that expectant mothers who are suspected of having contracted the Zika virus are monitored.
The actionable steps are to ensure that a state-level pregnancy reporting system is in place to actively monitor expectant mothers who are suspected of having contracted the Zika virus, and to introduce programmes dealing with training, counselling and advice to pregnant mothers and health care workers dealing with the pregnant mothers.
Step 7: Rapid Birth Defects monitoring and follow ups
The goal is to ensure rapid detection of microcephaly and other birth defects and to plan for adequate services for these children and families.
Step 8: Travel Health News
The goal under this step is to ensure that travellers who go to areas which are infected with the Zika virus receive the appropriate information regarding risks and preventative measures.
Step 9: Clinician outreach and communication
The goal is to keep healthcare practitioners updated as to the risks, recognition, diagnosis, reporting, clinical management and outcomes as well as prevention of the Zika virus infections.
The actionable measures would be to have reviews and update guidelines on the Zika virus as well as identify the most appropriate and functional channels to share information with healthcare providers.
Step 10: Risk communication / community education
The goal is to inform the public about Zika and related birth defects or illnesses, especially microcephaly and other harmful effects to women and their foetuses.
The actionable steps here are to develop communication messages with key partners and stakeholders and to identify local vendors who can assist in information dissemination on the Zika virus.
Conclusio
Monitoring, vector control, information and advice are all helpful. Even so, the Zika virus will continue to spread, and a vaccine is needed. It will take several years before the action of the virus is fully understood, potential vaccines developed and clinical trials completed.
Arvitha Doodnath, Legal Researcher, and Charles Simkins, Head of Research, Helen Suzman Foundation, 23 September 2016
[1] A vector is a means by which an infection is spread.

